Nourish Your Cycle: The Impact of Nutrition on Your Menstrual Health
Before we chat about nutrition and your menstrual cycle, let’s delve into what your cycle involves.
The menstrual cycle
Credit: Women’s Health Network
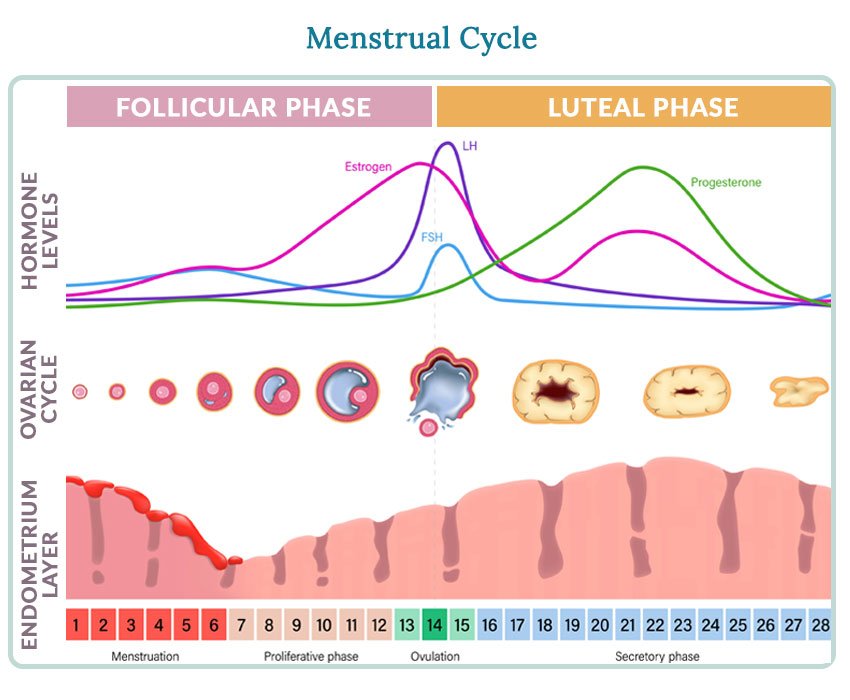
The menstrual cycle has 4 phases that consist of different hormonal and physical changes that prepares a woman’s body for pregnancy. The average length of a menstrual cycle is 28-29 days, although up to 35 days is still considered normal, as every woman is slightly different (Rosetta et al. 2017).
Phase 1: Menstrual. (Mihm et al. 2011)
This phase, commonly known as a period, lasts 1-5 days and is when the lining of the uterus, called the endometrium, is shed, causing bleeding. Oestrogen and progesterone are low during this time.
Phase 2: Follicular or proliferative.
This phase occurs from approximately day 6-14 in your cycle. Follicle stimulating hormone (FSH) is released and stimulates the ovary to produce around 5 to 20 follicles. These follicles stimulate the lining of the uterus to begin thickening for a potential pregnancy, and cause a rise in oestrogen and progesterone. Around day 10 of your cycle, a follicle will mature into an egg.
Phase 3: Ovulatory.
This phase occurs at approximately day 15-17, and signifies the release of the mature egg, or ovulation. This is triggered by the release of leutenizing hormone (LH) and FSH. Once the egg is released, it will survive for 24 hours. If the sperm reaches the egg during this time, the egg may become fertilised.
Phase 4: Luteal or secretory.
Days 18-28 of your cycle involve the development of the corpus luteum from the ruptured follicle. If there is no fertilised egg, the corpus luteum will die and menstruation will occur. If the fertilised egg does implant into the uterus wall, the corpus luteum ensures hormone levels and nutrition are appropriate for the embryo to develop.
Ovulation
Ovulation is a key aspect to getting pregnant as this is when the mature egg is released so the sperm can fertilise with it. Ovulatory dysfuction is when ovulation fails to occur (anovulation) or occurs on an infrequent or irregular basis (oligo-ovulation).
Factors affecting ovulation include:
Age
Alcohol intake
Hormone balance, including conditions like PCOS and hypothyroidism
Obesity
Low body weight
So you can see how each phase is critical for setting your body up for a successful pregnancy. Therefore, if you are not ovulating, or your hormone rise isn’t working at the right time, chances of a successful pregnancy are reduced.
So how does nutrition impact the menstrual cycle and ovulation?
The good news is that dietary modifications have been shown to improve ovulatory disorders that affect fertility. A large study of women without a history of infertility showed that a combination of 5 or more lifestyle factors were associated with a 69% lower risk of ovulatory disorder infertility (Chavarro et al. 2007).
Nutrition can have an impact on the changing hormone levels throughout the cycle, so there is more research coming out about how you can adapt your eating to the stage of your cycle. For instance, eating oestrogen supporting foods in the first half of your cycle, and then switching to progesterone supporting foods for the second half (stay tuned for future blogs coming on these topics).
As mentioned above, there are certain factors that can impact ovulation which can be improved through dietary changes. For example, managing elevated androgens such as testosterone in PCOS, through including a cup of spearmint tea daily, can help improve chances of regular ovulation (Grant, 2010).
For women without a period, strategies like eating more healthy fats to increase body weight and therefore improving hormone production is critical.
It’s important to remember that resumption of ovulation could take up to one year or longer once dietary changes start to occur (Scofield et al 2012).
What should I change in my diet?
Everyone is very different when it comes to their menstrual cycle. It’s important to track your cycle and understand whether you are ovulating or not, if you have an appropriate luteal phase, and whether your cycle length is consistent and appropriate. Then, depending on your medical history, lifestyle, and dietary patterns, a plan can be tailored. Unfortunately it is hard to give a cookie cutter approach as there are so many different aspects that could be affecting your cycle.
Instead, I’d recommend booking an appointment with a fertility dietitian to tailor a plan to you and your circumstances. That way you know you are on the right track to restoring a natural cycle, and on the road to getting pregnant! If you’re keen to get started today, book in for a FREE discovery call here, and we can chat about what might work best for you!
References
Scofield KL, Hecht S. Bone health in endurance athletes, runners, cyclists, and swimmers. Curr Sports Med Rep. 2012. 11(6):328-334.
Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol. 2007. 110(5):1050-1058.
Grant P. Spearmint herbal tea has significant anti-androgen effects in polycystic ovarian syndrome. A randomized controlled trial. Phytother Res. 2010. 24(2):186-188.
Rosetta L, Thalabard JC, Tanniou J, Ducot B, Maitrot-Mantelet L, Rousset-Jablonski C, et al. Ovulatory status and menstrual cycle duration assessed by self collection of urine on pH strips in a population-based sample of French women not using hormonal contraception. Eur J Contracept Reprod Health Care. 2017;22(6):450-8.
Mihm M, Gangooly S, Muttukrishna S. The normal menstrual cycle in women. Anim Reprod Sci. 2011;124(3-4):229-36.